Cancer cells are often described as “abnormal,” but if you are not familiar with how normal cells behave, it can be difficult to understand what exactly abnormal means. When it comes to cancer cells vs. normal cells, there are numerous differences.

Stories of progress, inspiration, and information in overcoming osteosarcoma.

Cancer cells are often described as “abnormal,” but if you are not familiar with how normal cells behave, it can be difficult to understand what exactly abnormal means. When it comes to cancer cells vs. normal cells, there are numerous differences.
First, while normal cells need signals to tell them to grow and divide, cancer cells can do so without any external signal. They also ignore signals that cause healthy cells to stop growing or die.
Cancer cells can invade nearby tissue and even travel to other parts of the body, whereas normal cells mostly stay put and stop growing when they encounter other types of cells.
Even more challenging, cancer cells can hide from the immune system, and in some cases, they can even trick the immune system into keeping them safe. They also can cause blood vessels to grow towards them, providing them with food and oxygen. Some cancer cells even create their own sources of energy.
While normal cells contain two copies of nearly every gene, cancer cells often have additional or missing chromosomes in their DNA. Most childhood cancers look almost normal at the genetic level, but simple genetic alterations can cause widespread changes in gene expression that lead to cancer. The chromosomes in osteosarcoma cells, however, can be described as “chaos,” according to Ryan Roberts, MD, PhD, a physician and osteosarcoma researcher at Nationwide Children’s Hospital and an assistant professor of Pediatrics at The Ohio State University.
“Osteosarcoma is really distinct from almost all other pediatric cancers in that you might have 15 copies of this gene and one copy of that gene and no copies of another gene,” he says. “It just looks like you took all the genes and put them in a blender.”
The good news is that scientists continue to study osteosarcoma cancer cells vs. normal cells and are learning more about them every day.
“We have had an explosion in our understanding of the basic biology of what makes osteosarcoma malignant and what makes those cells behave differently from normal bone cells,” Dr. Roberts says. “We understand osteosarcoma so much better than we did 15 years ago. That is not to say that we understand it well, but we understand more than we did — and that is a reason to be optimistic.”
One area of osteosarcoma research that makes Dr. Roberts optimistic for the future is a type of targeted therapy called antibody drug conjugates (ADCs). ADCs combine the power of chemotherapy with the precision of immunotherapy.
“Thanks to work done by Dr. Richard Gorlick’s lab and others, we have identified proteins that osteosarcoma cells express on their surface, but that normal cells do not. This makes for some promising new antibody targets,” Dr. Roberts says. “Researchers are putting that together with drugs that are actually highly toxic, which is okay since we can now direct them straight to the tumor cells.”
So far, Dr. Roberts says, trials of ADCs have been highly effective in animal models. The next step will be testing them in human patients, which he hopes the osteosarcoma community will begin in the coming year or so.
Another area of research that excites Dr. Roberts involves identifying the DNA signatures unique to each osteosarcoma tumor, which scientists are now using to predict how a tumor will behave, such as whether or not it will respond to certain therapies.
“This is really exciting because there are direct implications for how we should design clinical trials and how we should identify patients that should be assigned to certain types of treatments,” Dr. Roberts says. “It is a concrete way of stratifying patients into groups so that we can customize their therapy.”
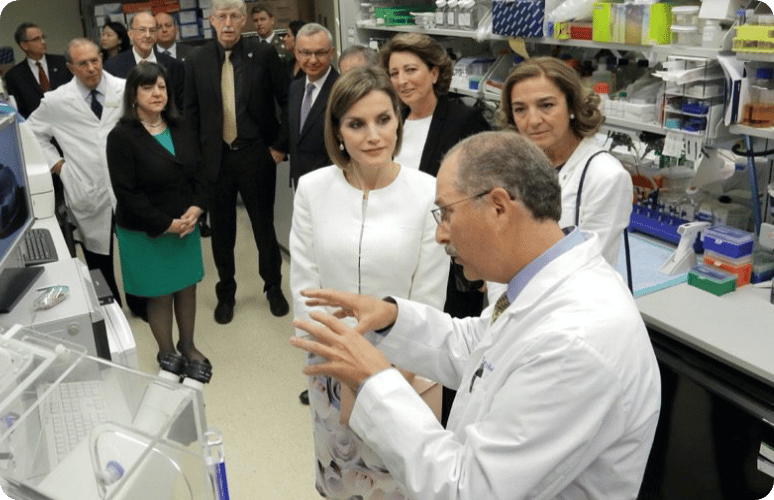
The third area of research Dr. Roberts is especially optimistic about comes from his own lab (pictured above at a team retreat).
“My lab has focused on understanding why it is that osteosarcoma loves to grow in the lung but not really anywhere else,” he says.
What Dr. Roberts and his team have discovered is that there are particular pathways that can be activated between these tumor cells and lung tissues that allow osteosarcoma cells to survive where other types of cancer cells typically die.
Better yet, Dr. Roberts’ lab has already identified existing drugs that effectively eliminate metastatic lung lesions in animal models.
“It is not FDA-approved yet, but it is being used in other clinical trials,” Dr. Roberts says. “So that, too, is something we are working on getting into clinic sooner rather than later.”
With so much promising research on cancer cells and how they spread happening, Dr. Roberts says he thinks osteosarcoma treatment could potentially look very different in five years’ time.
“We are fortunate that we have so many good ideas now in this space,” he says. “With a growing number of good ideas and a limited number of patients with the disease, the challenge becomes prioritizing testing those ideas in patients in order of likely impact.”
Stay informed as we work to identify new treatments for osteosarcoma.
We never sell or share your information.
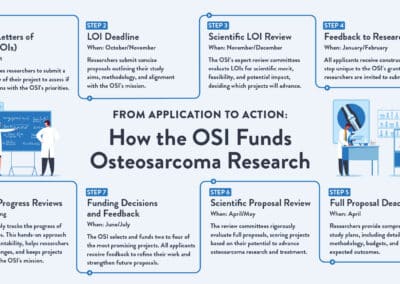


Your donation provides immediate and long-term support to osteosarcoma patients.
Sign-up for our newsletter and stay up-to-date about our fight against Osteosarcoma!