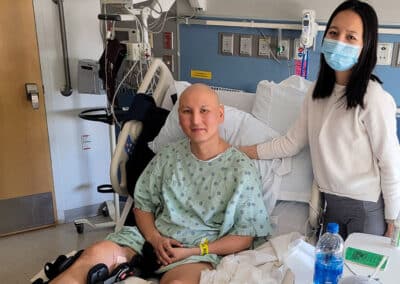
A teenage osteosarcoma patient had a clear vision of her end-of-life plan. She wanted to be at home, in her own bed, listening to Taylor Swift, with family and friends around her reading her favorite church hymn.
And then one day, she fell in the shower and became unconscious. She was rushed to the hospital, where she had a breathing tube inserted. This was so far from what she had wanted for her final hours, and her family did everything they could to honor her wishes anyway. They decorated her hospital room so it looked more like home. They invited her pastor, friends, and family to surround her hospital bed and read her favorite hymn. They put Taylor Swift on in the background. After the nurses removed her breathing tube, she opened her eyes and whispered, “Thank you.” Then she took her last breath.

In her work as a palliative care specialist, Dr. Rosenberg provides many forms of support to families facing a child’s serious illness.
The Frontline spoke with Dr. Rosenberg about one of the hardest dimensions of her work: preparing families for end-of-life conversations.