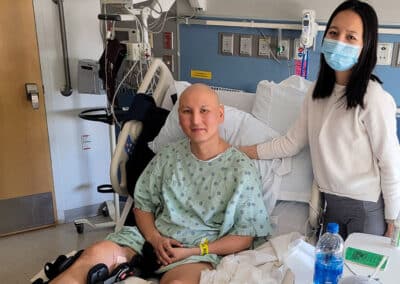
When a child has a serious illness, both the child and their family are bombarded by the demands of the illness — doctor’s appointments, treatment regimens, and difficult decisions to make — all while surrounded by a cloud of uncertainty. Palliative care can be an extra layer of support.

“These can be the worst moments of people’s lives, and they deserve to have everybody around them providing support,” says Abby R. Rosenberg, MD, Chief of Pediatric Palliative Care at Dana-Farber Cancer Institute and the Director of Palliative Care at Boston Children’s Hospital. “We in palliative care want to help provide that support.”
The Frontline spoke with Dr. Rosenberg to learn how pediatric palliative care helps children and their families navigate life-altering illnesses like osteosarcoma.