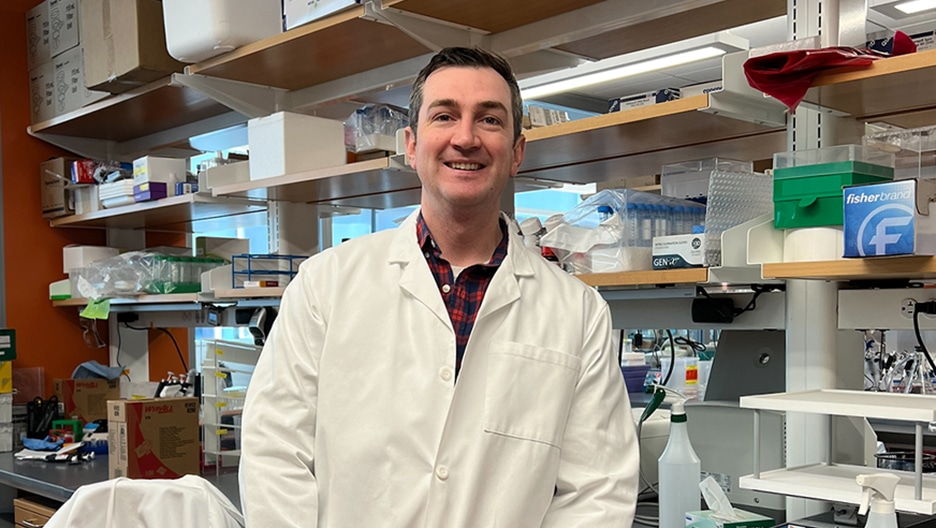
Cancer is more difficult to treat once it has metastasized or spread beyond its original location. Metastatic osteosarcoma in particular, which accounts for about 20% of osteosarcoma diagnoses, is especially challenging to treat, since the disease often spreads to the lungs. Researcher and oncologist James Morrow, MD, PhD, is on a mission to change how metastatic osteosarcoma is treated so patients will survive.
While completing graduate studies at Case Western Reserve University, Dr. Morrow was awarded a 2011–2012 Howard Hughes Medical Institute fellowship, allowing him to study tumor metastasis in the lab of Chand Khanna, DVM, PhD. (Dr. Khanna serves as Strategic Advisory Board Chair at the Osteosarcoma Institute.)
Building on this research, Dr. Morrow joined the lab of Peter Scacheri, PhD, at Case Western and published a 2018 study in Nature Medicine describing the role that gene enhancers play in tumor metastasis. Today, as a clinical fellow at Dana-Farber Cancer Institute in Boston, Dr. Morrow splits his time between his osteosarcoma research and treating young patients in the clinic. The Frontline sat down with Dr. Morrow to learn more about what is on the horizon for treating metastatic osteosarcoma.
Can you explain what metastasis is and what role it plays in osteosarcoma?
Metastasis is the process by which cancer cells that are initially in primary tumors leave those tumors and spread to other parts of the body. Cancer in general, and osteosarcoma in particular, is much more difficult to treat once it has metastasized.
The statistics are sobering. Patients who present with metastatic disease do not achieve cures about 70% of the time, whereas patients who present without metastatic disease do achieve cures about 70% of the time. My work treating patients serves as a critical motivator for my research, because I see firsthand the impact that new approaches to treatment can have for individual patients and their families.
Can you share your research involving gene enhancers and how they are connected to metastasis?
Think of gene enhancers as switches that turn on or dial up gene expression. They are not genes themselves, but they are the key drivers of cell identity. In any given cell type, there could be tens of thousands or hundreds of thousands of gene enhancers that form a sort of circuitry in the cell.