How Is Quality of Life Measured?
Quality of life is unique to each individual, Dr. Helman explains. Quality of life indicators can include physical well-being, emotional health, spiritual needs, social connections, and personal goals.
To evaluate quality of life, health professionals use standardized questionnaires and assessments. These questionnaires — which are tailored to the patient’s age — consider health-related quality of life aspects such as pain levels, fatigue, and physical functioning, as well as emotional well-being and social support, says Dr. Helman. These assessments provide valuable insights into a patient’s experience and can guide treatment decisions.
“These measurements need to be given in intervals throughout a patient’s treatment journey,” adds Dr. Helman. “This allows their care team to assess how the treatment is affecting the patient’s life on both a physical and emotional level.”
Age Makes a Difference
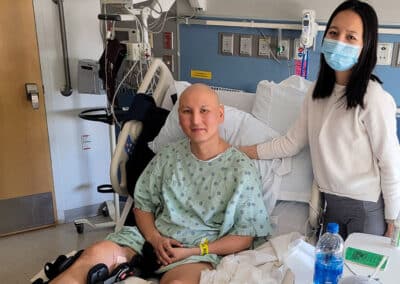
Quality of life in healthcare differs for everyone, but these differences become more pronounced when comparing adults, children, and young adults with cancer.
Adults often prioritize maintaining independence, managing symptoms, and preserving social connections.
Meanwhile, children require a different approach that considers their developmental needs, school attendance, sports and activities, and family dynamics. Play, education, and maintaining a sense of normalcy are critical components of a child’s quality of life.
On the other hand, adolescent and young adult (AYA) patients are finding their voice when it comes to making treatment decisions and body autonomy. They might be considering things like living independently for the first time, going to college, or starting a family.
Asking the Right Questions
There are many questions to consider when balancing treatment decisions and quality of life. Here are some to ask your providers:
- How will treatment affect how I feel (physically and emotionally) each day?
- Will I be able to go to work and/or school?
- Will my treatment leave me immunocompromised?
- How long will treatment last?
- Will I be able to remain active and take part in sports and/or activities?
- Should I consider palliative care and other supportive therapies?
Another important consideration is the financial burden associated with a cancer diagnosis, says Lori Wiener, PhD, a licensed clinical social worker and senior associate scientist in the Pediatric Oncology Branch of the National Cancer Institute. Dr. Wiener explains that treatment-related costs, nonmedical out-of-pocket expenses, income loss, and travel costs can all contribute emotional distress and decreased quality of life. She encourages patients and families to ask oncology social workers about financial resources so they can access the care they need.
Finding Support
As you advocate for yourself and navigate competing priorities, remember to lean on your support system. Seek emotional and social support from loved ones, join support groups, and consider quality of life services like counseling. “No matter how old a patient is, or how dire their case, I always recommend they seek some form of counseling during and after treatment,” says Dr. Helman. Dr. Wiener recommends financial assessments and counseling throughout the treatment trajectory.