“At first, the immune system is really trying to fight it, but it gets completely overwhelmed. The immune system then contributes to the problem by activating the part of the body that is trying to heal,” says Dr. Kaplan.
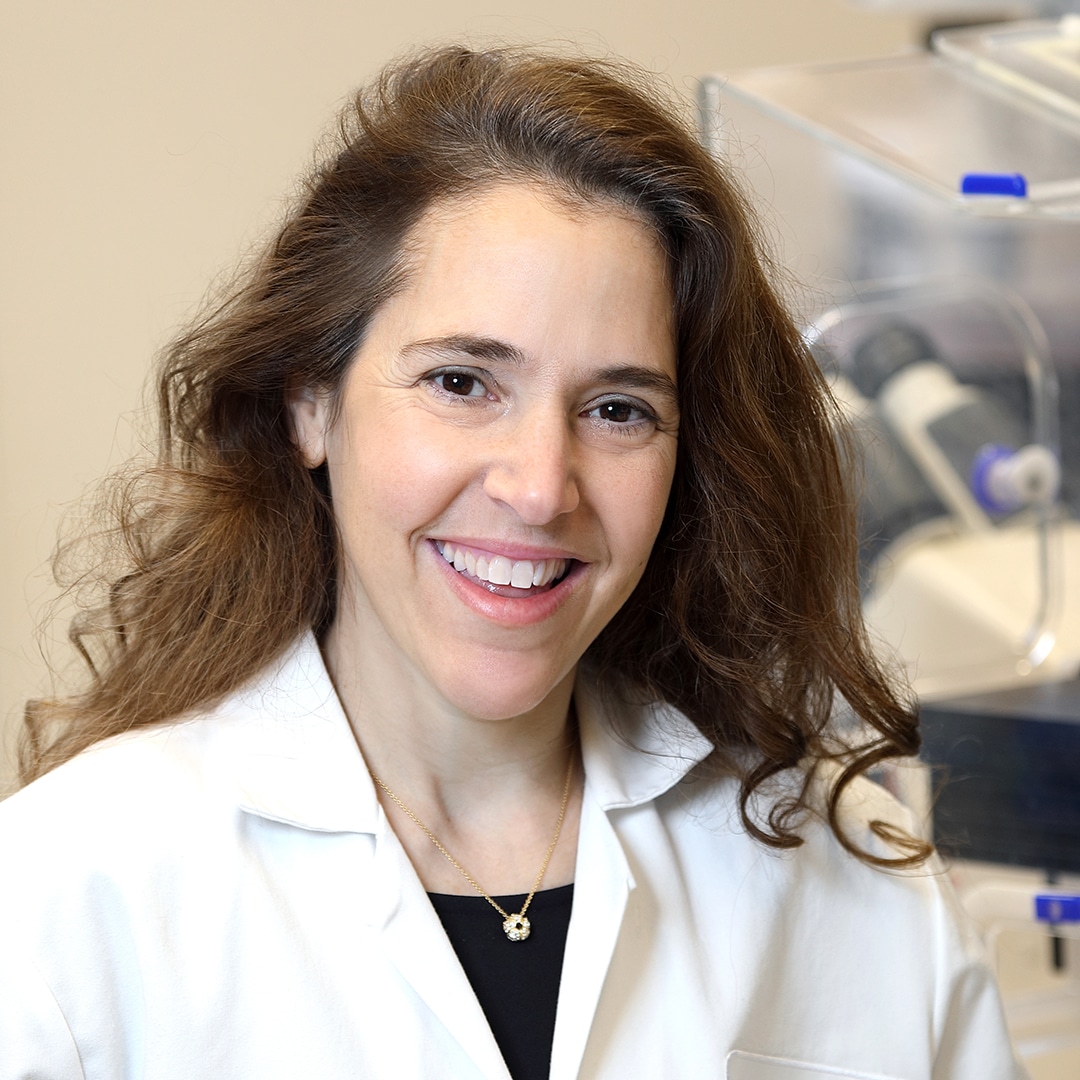
Zooming in on the “Mom Cells”
The specifics of Dr. Kaplan’s research will be the subject of a future article, but the basic premise is that the non-tumor cells and matrix in the cancer have a very important role in cancer development, growth, and spread. These cells and matrix communicate and organize to make the cancer cells better able to survive, resist treatment, and persist in a new environment. Too often, the body’s injury repair response makes cancer worse.
One area of Dr. Kaplan’s research focuses on myeloid cells, which she terms the “moms” of the immune system. Much more focus has been on T cells since they have the ability to directly kill tumor cells or cells infected with virus or bacteria. The myeloid cells are a group of very fluid, adaptable cells holding many different jobs in responding to infection or injury. “They suss out danger and are the first to respond to a problem. They are the last to leave the party, and they clean everything up.” Myeloid cells eat up cells that are dead, damaged, or mutated. They also travel through the bloodstream to rally other cells to address the problem area when they detect injury, damage, or infection.
This rapid communication may be the reason that osteosarcoma can metastasize to distant parts of the body, moving from a bone in the leg or a shoulder to the lung or another bone, for example. Dr. Kaplan’s team has found that osteosarcoma is chock full of myeloid cells. Dr. Kaplan is attempting to genetically engineer myeloid cells to help instruct the T cells and NK cells to kill cancer, instead of fueling cancer by telling the T cells and other cells to stand down.
“When I first started studying myeloid cells, endothelial cells, and stromal cells with David C. Lyden, MD, PhD, very few people cared about the microenvironment — they were very focused on the genomics of the cancer,” says Dr. Kaplan. “Genomics of the tumor is critical — it is like the foundation of the house — but you also need to know what the rooms look like.” Through her research, she hopes to illuminate a key element of cancer metastasis to ultimately create more effective osteosarcoma therapies.